When Amy Smyth and Sharon Hughes-Magill were given the news they had heart failure, their lives as they knew them changed in an instant. This week marks World Heart Day (29th September), and Amy and Sharon are sharing their stories in support of Northern Ireland Chest Heart & Stroke’s (NICHS) current heart failure awareness campaign. The campaign aims to increase public awareness of the condition which can have worse outcomes than many cancers. Amy and Sharon hope speaking out will help put a spotlight on heart failure, its symptoms, and encourage people to seek medical advice if they are experiencing any signs of the condition.

Amy’s Story
Amy, from Armagh, was told last year she has heart failure, at the age of just 32. The news came as a devastating blow after Amy had already been on a difficult journey with her heart health, as she explains; “When I was told I had heart failure, I couldn't comprehend what the doctor was telling me. I didn’t know anything about heart failure. I had maybe seen it on TV and to me, heart failure was the end of your life, so it was terrifying. When I got the news, I felt like I was being dragged down again, after everything I had already been through.”
In 2022, Amy suffered three heart attacks and was diagnosed with a rare heart condition called Spontaneous Coronary Artery Dissection (SCAD) which is when a tear happens in the wall of a coronary artery. This all came completely out of the blue for Amy; “I had never had any issues with my health, certainly not with my heart. I was only 31, and my little girls, Fianna and Róise, were 2 and 3 years old at the time so it was an unbelievably frightening time.”
“I had been to see my GP because I had experienced pains in my chest and left arm and felt nauseous and dizzy one day. Believe it or not, none of those things registered with me that it could be something serious. I just didn’t think that was a possibility because of my age and general health but my doctor sent me to Craigavon Area Hospital A&E. I had tests done and then saw the Consultant Cardiologist who told me I’d had a heart attack, and I just couldn’t believe what I was hearing. She told me my troponin levels were over 3000 and 14 or more shows you have had a heart attack. I was in total shock.”
“I ended up in hospital for a week as I needed to have a procedure called an angiogram which is a heart test that looks at the blood supply of your heart, but the ward’s machine was broken, and they were waiting on parts to fix it. I was having small niggles here and there but generally felt ok and was up walking about. One night however I had another heart attack, and the pain was unbearable. You would think having a heart attack on the cardiology ward means you’re in the right place, but they still had no angiogram machine which meant there was little they could do, so I was blue-lighted in an ambulance to the Royal Victoria Hospital in Belfast.”
Amy continues; “When I was having the angiogram there, the Consultant told me my artery was blocked but it was nothing to do with plaque or my cholesterol, it had spontaneously torn open and that this condition was called SCAD. I just couldn't get my head around what he was telling me.”
“I had a procedure called a PCI and a ballon was inserted into my artery to blow it open again. After the procedure I was on complete bed rest. I was afraid to even cough or sneeze and it was terrible. A few weeks later I went back to work as a Care Manager and 16 weeks after that I started to feel chest pain again one evening. It wasn’t like the pain I felt before and I thought ‘it's not a heart attack because I know what a heart attack is like now.’ I went to bed that night but the next morning I still didn’t feel right so I went to the hospital. Once again, my troponin levels were sky high, and I was told I’d had another heart attack.”
“I was once again sent to the Royal Victoria Hospital for an angiogram which showed I’d had another SCAD, but on a different artery. I had another balloon PCI, and I was in hospital for a week. Again, I went back to work and at the start of January 2023 I went to my doctor because I was not feeling at all well. I was exhausted, completely drained, and was short of breath but I put that down to the fact that I’d had 3 heart attacks! I was still working full-time because as a single parent of 2 young children I had no other option, I had to just get on with it.”
“I had bloods done and the doctor told me my BNP levels were over 900. She explained that anything over 400 would be an indicator that you are in heart failure and the higher number, the more severe your heart failure is. I came out of that appointment feeling dizzy, like I was going to be sick. I had to get my phone out and Google heart failure as I didn’t understand what I was dealing with. I’d already had the trauma of being diagnosed with SCAD, that was enough, but to have heart failure on top of that. I just couldn't get my head around it.”
Amy was then sent for further tests and explains; “I went for an echocardiogram a couple of days later and it showed my heart function was at 40%. I had to go again eight weeks later and by then my function had gone down to 35%. I was expecting a situation of ‘you have been diagnosed with this, but you are going to get better’, but I was getting worse. I have always had low blood pressure, and the heart failure medication knocked me for six, it was horrendous. The heart failure team explained the medication is designed to take as much pressure off your heart as possible, but it really affected me. Before the medication I was absolutely exhausted, but once I was on it, I couldn't function, it made me 100 times worse. But the team worked with my medication to get it to a level that works for me and that I can manage.”
“Again, I continued working until December 2023 when I literally couldn't do it anymore. I couldn't function in my day-to-day tasks of getting the children to school, getting myself to work, the rush of the motorway, things you would never think twice about. By that stage I had no quality of life, I was exhausted all the time, and it was horrendous. I had to stop working. I had never had a chance to heal after everything- I had battled on after getting this life-changing diagnosis and both the physical and mental impacts of that were huge, it took its toll on me.”
As the months have passed, Amy is feeling a bit more settled as she explains; “I have had time to read up and learn about my condition and I’ve had time to rest. Beforehand, it felt like a death sentence. My first reaction was, ‘heart failure, that means my heart is going to die, how long do I have left?’ I felt like I had a timer on me. I did lots of my own research however and that moved me away from that thinking and I realised, although it isn’t curable, heart failure was not the end of my life, I could learn to live with it.”
“That is why I’m supporting Northern Ireland Chest Heart & Stroke’s campaign, to spread awareness and help people understand heart failure better. To understand what it means if they, or a family member or friend, get a diagnosis. There is often a lot of jargon used in medical settings and I want to play my part in helping people break through that and understand what heart failure is. There are so many people affected by the condition in NI and more will be, so it’s something people need to be aware of and we need to be talking about more.”

“I also want to highlight that heart failure can affect people of any age. I am only 33. People assume heart failure only affects people in their seventies and eighties but that’s not the case. The prognosis for younger people can also be hugely different and that’s something I really want people to understand. You can’t stick one diagnosis and one prognosis onto everyone. It’s so important that anyone of any age who is experiencing any potential signs of heart failure, or any other cardiac condition, are aware and get things checked out.”
Even though Amy is on medication, she suffers from symptoms of heart failure every day. “I'm exhausted most of the time, I’m short of breath and I can’t begin to explain the impact this has had on my life. It was horrible for my children to see me having to go to hospital and have procedures and now I just don't have the same energy for them. They are only 4 and 5 years old and that is heartbreaking.”
“I met my partner, James, after my diagnosis, and our relationship is different because of it. My children, go to bed at 6.30/7pm and I have to go to bed after them. I can't function after that sort of time and he’s very understanding of that, but it affects me mentally as I feel bad about it.”
“I'm only 33. My friends will be going out going for a drink or a meal and that's just completely out of the question for me. Those might sound like silly things, but it's more the fact the choice has been taken away from me. Heart failure completely rules everything in my life and that’s the reality of it.”
“The exhaustion is hindering but my anxiety is bad too, so I struggle to actually get to sleep. That's when the worry starts to kick in for me, when I’m lying in bed, exhausted, trying to get to sleep. The reality of it all kicks in and it’s terrifying at times. The mental impact is as tough as the physical impact.”
“As they say however, time is a great healer and as it goes on, I’m dealing with things. This has changed me in so many ways but I’m trying to be positive and am moving on with my life as it is now as best I can.”

Sharon’s Story
Sharon, 45, from Newry, was given her heart failure diagnosis two years ago, and like Amy, it was the culmination of a lengthy battle to discover what was causing her health problems. Sharon recalls; “It all started in 2021. I was having difficulty with breathing and didn’t know why. I had started my studies to be a social worker and people pointed out my breathlessness, but me being me, I just thought I was doing too much. I was always on the go and loved being busy. That Christmas I developed Covid symptoms but didn’t realise there were deeper issues going on. I rushed to get back to normal as I was starting my social work placement and tried to just get on with things and push through.”
“I lost my mother-in-law in April 2022, and I was arranging her funeral when I went to my GP Practice Nurse for something routine. The nurse noted my breathing and was concerned. A doctor assessed me and that led to me being blue-lighted to hospital. I have asthma and they thought it was something to do with that, so I was given asthma treatment and was discharged later that day to prepare for the funeral.”
“The following week I was sent back to hospital as I was still struggling to breathe. I was admitted overnight, and again I was treated for my asthma and sent home. I went back to my GP a week or two later and told her I was getting no better and was struggling with everything, even walking to the bathroom was an ordeal. She decided to screen for clots, and when the results came back, I was sent straight to A&E for a CT scan. This showed I had ten clots between both my lungs which was a complete shock. I started treatment and thought I would see big improvements, but I found I was still struggling, my breathing wasn't getting better, and I was experiencing chest pain. I was referred to the Chest Pain Clinic and was being treated for angina whilst waiting for a CT scan of my heart. Fast forward to the September 2022 and I was finding things were getting no better, I was fatigued and struggling to do simple things such as dressing. I was unable to work and needed to take time off from my degree. I went back to my GP with the chest pain, and she sent me to the hospital, concerned I had unstable angina. I was admitted to Coronary Care Ward for further testing and following an echocardiogram was told I was in heart failure.”
Sharon continues; “The doctor said to me, ‘heart failure isn’t the death sentence it used to be’, but that just made me think it must be a death sentence. I was very frightened, and my world felt lonely. I was left thinking, ‘why has this happened to me?’. I had so many questions as to why because I don't smoke, I'm not a big drinker, there was no obvious reason for it, and still, nobody can give me a reason. I started Googling heart failure and learnt it is a life-limiting condition. The website I was on gave a prognosis of five years and I was thinking, ‘how do I prepare my family? How do I do this?’. I have four children, and they and my husband were really frightened about what might happen to me. The way I was told I had heart failure didn’t give me more information about the condition, what treatment plans might look like and so on and that could have been dealt with a lot better.”
“In terms of treatment, I was put on medication when I was in hospital. I was at what they call the optimal dosage, but things have been up and down with my medication because of other bouts of illness which has meant things have had to be changed. It has been a bumpy road trying to get to a stable place with my medication which has been unsettling too. Even now I’m still not there and things are changing.”
“I also went to Cardiac Rehab and that helped as I learnt what my limits are. Not all heart failure patients get this however, it depends on what Health Trust they are in, and that just isn’t fair as cardiac rehab is so important for managing heart failure. I hope that will change.”
Sharon battles extreme fatigue on a constant basis because of her heart failure and this has had an enormous impact on her day-to-day life as she explains; “Nobody realises what true fatigue is like unless they have something like heart failure. I had experienced exhaustion before, but this is hitting walls that you just can’t get over and people do not understand.”
“Most days I am in my bed at 6.30/7pm as I have no energy by then. I am in bed before my children. I can't give anything more at that stage and it's awful because my husband comes home from work and we're not getting any time together. I'm so lucky that I have such a good husband, and he completely understands but I feel frustrated for him.”

“I am going into the third year of my degree after I had to take time out during my second year because of my heart failure. I have to provide evidence I have the condition just so a placement closer to home can be considered for me. Working, studying, and traveling five days a week is exhausting, and people just don't understand the impact heart failure has on the body. My body works so much harder, I’m out of breath after what seem simple tasks, and that is very hard and frustrating.”
“My daughter has asked me why I don’t give up working and studying but I’m not ready to give up. I am still young. The reason I'm continuing my social work studies is because I can't do my current job anymore. I work in supported living for people with learning disabilities and physically I'm not able to do it. I've been pushing on with my studies because I need this, it is something I’ve wanted for years. One of my prayers is for me to be able to finish my studies so that when I do leave this world, I can say that I have given it everything. I’m not thinking morbidly but I just don't want to have regrets, that is really important to me. I keep focussing on graduation and the hope that down the line I will be able to help people going through something like what I am.”
Sharon continues; “I don't want to lose who I am just because I have heart failure. I can't let heart failure win; it’s not going to beat me. Being determined is probably a good thing for dealing with heart failure but at the same time it is hard for me to go slower and easier and take time to rest and recharge. I am not that kind of person. My doctors have said to me, ‘many people who have been where you are would have given up Sharon, but you just keep going’. That’s my mantra; keep going. Stopping isn’t who I am.”
“Fatigue isn’t the only side effect I suffer from. I also experience a lot of pain in my legs, joints, and toes. I'm constantly freezing. I have brain fog and forgetfulness because of the fatigue. I've had to move to sleeping downstairs and on the days I'm really tired I have to use a shower chair.”
“I am only in my forties. Never in my wildest dreams did I think this would happen to me. It’s a real battle but I still need to get up every day, sort the children, get to work, and I think that’s the best thing for anyone with heart failure, to still have a purpose. You need to find something that will make you get up in the morning because you could just give up but it's important not to. You need to find your own level of ability and still find happiness.”
Like Amy, Sharon is supporting Northern Ireland Chest Heart & Stroke’s heart failure campaign to spread awareness of the condition and its signs. “I had no clue about the signs of heart failure. I also think because I was being treated for asthma and clots initially, nobody thought to look at my heart and I wonder if that had of happened earlier if things might be different. It is important for medical professionals to be more aware of heart failure as well as the public. There isn’t enough information about heart failure, and I think what NICHS are doing with their campaign is great. Spreading awareness of the signs and symptoms, educating people, hopefully getting people diagnosed as early as possible so they have the best possible outcomes. Also educating people that it is something that can be lived with and it’s not a condition that only affects older people.”
The impact of her diagnosis has been massive for Sharon but also for her family as she explains; “It has been so hard for my children and family. My youngest child is 8 and when I told him about my heart failure he said, ‘but Mummy, you're not going to die, are you?’. That was heartbreaking.”
“The whole family goes into turmoil after a heart failure diagnosis and sometimes we feel like we’re drowning, and we don’t know where to turn. The support available to families needs to change for the good of the mental health of everyone. When people have a cancer diagnosis for example, there is much more support around talking to people about it and dealing with things as a family but there is nothing like that for heart failure and it can have worse outcomes than many cancers.”
Sharon concludes; “Everything has changed for me because of this condition, and it is frightening. There are times when my breathlessness or palpitations are so bad I ask myself, ‘will I see my 50th birthday?’, and that's awful. That fear has made me slow down, however. I am going to be a grandmother for the first time soon and I want to be here for my grandchild and to see my children grow up. I want to be able to have that time. It’s not that I want to slow down, it’s now a necessity to slow down.”
“The biggest thing that I’ve learnt from this is life is short and that we need to make time for the important stuff. For me it’s all about making memories now and I want the children to remember the good times. For example, we have never had a family holiday and next year we are determined to have one.”
“I grieve for the person I used to be, for the work I used to do but my family keeps me going. That helps me deal with this new life, but accepting this is the new life is the hardest part. I think anybody who is diagnosed with a serious condition goes through a stage of grief. We are still alive, but we are grieving for what life should have been. I’ve just had to learn to keep getting back up when I’ve been knocked down; and I will keep getting back up.”
Ursula Ferguson, Director of Care Services at Northern Ireland Chest Heart & Stroke, comments; “We are so thankful to Amy and Sharon for sharing their powerful stories in support of our heart failure campaign and helping us raise much-needed awareness of the condition.”
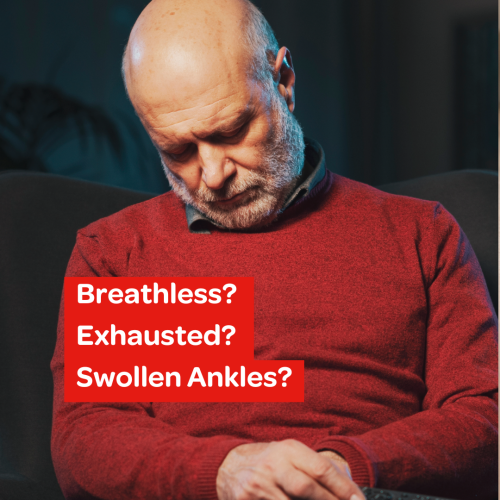
“It is estimated there is likely to be an increase in people being diagnosed with heart failure in excess of 50% in the next 25 years and this is a great cause of concern for us. It is crucial people are aware of the signs of heart failure. The most common symptoms are breathlessness, exhaustion, and swollen ankles. If you are experiencing any of these symptoms, we would urge you to make an appointment to speak to your GP as soon as you can. If you do have heart failure, the sooner it is diagnosed the sooner you can get started on the correct treatment and care plan which is vitally important.”
“If you are living with a heart failure diagnosis, the important thing to remember is the condition is treatable and manageable. NICHS’s Care Services team are also here to provide support through our Family Support Service, our Heart Strong Education Programme, and our Taking Control Self-Management Programme. You are not alone and NICHS is here for those who need us.”
Our Heart Failure Awareness Campaign
In a recent survey, 66% of people in NI did not know the symptoms of heart failure.
We have launched our new Heart Failure awareness campaign as it's vital that everyone knows the symptoms to look out for and to get it checked if they think they may have any of the symptoms.
