Heart Failure can have more serious outcomes than many cancers.
However, in a recent survey, 66% of people in NI did not know the symptoms of heart failure.
It's important to know the symptoms as, like with many cancers, detecting heart failure early is crucial.
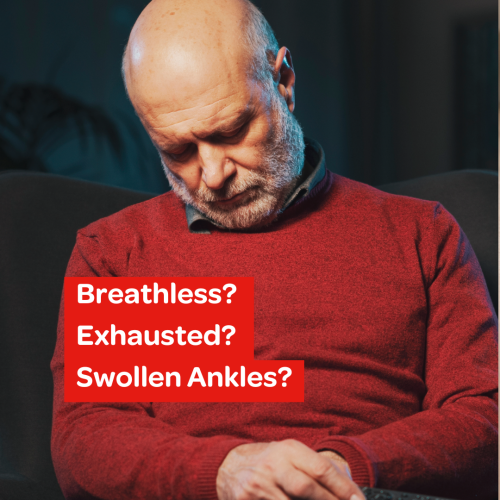
Symptoms of Heart Failure
The main symptoms of Heart Failure include:
Breathlessness
Exhaustion
Swollen Ankles
Other symptoms can include:
A persistent cough, or a cough that gets worse at night when you lie down.
Waking up from sleep feeling short of breath
Wheezing
Feeling lightheaded or dizzy
Palpitations, or feeling aware of a fast or irregular heartbeat
Loss of appetite
Rapid weight gain
Gradual, unintended weight loss
A bloated stomach
Symptoms may develop quickly (acute heart failure) or gradually over weeks or months.
Make an appointment to speak to your GP as soon as you can if you experience any of these symptoms.
This is important because if you do have heart failure, the sooner it is diagnosed the sooner you can get started on the correct treatment and get the right care.
If you have sudden or severe symptoms, call 999 for an ambulance or go to your local Emergency Department.

What is Heart Failure?
Heart failure (HF) occurs when your heart becomes too weak or stiff to pump enough blood around the body in the way it should.
When it is working normally, the heart relaxes to let it fill with blood, and squeezes to pump blood to meet all of the body’s needs. If it cannot fill and or pump properly, it becomes inefficient, and fails to do all the work that we need it to do. This causes symptoms such as breathlessness, fatigue and fluid retention.
Heart Failure is a long-term condition, and left untreated, symptoms get worse over time. However, with the right treatment, it can be managed, and the symptoms can be controlled for many years. Heart Failure does not mean your heart has stopped working completely – it just needs treatment and support to help it work better.
Real Life Heart Failure Stories
Find out more about Heart Failure:
-
A heart attack is caused by coronary heart disease. This is when there is a narrowing in one or more of the blood vessels that supply blood to the heart muscle. This narrowing is caused by fatty deposits (plaque) on the wall of the blood vessels. These plaques can rupture (burst), and when this happens the blood supply to the heart is cut off and this can cause damage to the heart muscle.
A cardiac arrest is when the heart suddenly stops beating, leading to a sudden collapse. The person will be unconscious and will need CPR.
Heart failure is when the pumping function of the heart is reduced because it does not squeeze or relax properly.
-
Heart Failure is often the result of a number of problems affecting the heart at the same time.
Causes of heart failure include:
Coronary heart disease
Heart attack
High blood pressure
Cardiomyopathy (disease of the heart muscle)
Irregular heartbeat or heart rhythm problem (arrhythmias) like atrial fibrillation (AF)
Damage or problems with the heart valves
Congenital Heart Disease (heart problems that occur at birth)
Overactive thyroid
Alcohol or substance abuse
Obesity
Anaemia
Endocarditis (a viral infection of the heart muscles)
Cardiac Amyloidosis (a build-up of abnormal proteins)
Pulmonary hypertension (high pressure in the lungs)
Some cancer treatments such as chemotherapy
Pregnancy
All these conditions can damage or put extra strain on the heart over a long period of time. The heart initially tries to cope with the extra workload by getting bigger, developing more muscle or beating faster to keep up with demand, but eventually it will fail to cope and symptoms will become evident.
-
When you visit your GP, the doctor will ask you a number of questions about your symptoms and medical history. Your GP will also listen to your heart and chest and check your blood pressure. If your doctor suspects that you have heart failure, they will check a blood test called a BNP. If the BNP comes back raised (abnormal) you may be referred to hospital for more heart tests such as:
An ECG (Electrocardiogram) - this test which records the rhythm, rate and electrical activity of your heart.
Chest x-ray - to check for fluid in your lungs or other lung conditions, or if your heart is enlarged.
An Echocardiogram. This is a scan of the heart that checks the pumping function of the heart. It also looks at how well the heart valves are working. This test is usually done as an outpatient. If the results of the scan show a problem with the pumping function or the valves, a referral will be made to a local heart failure team to have treatment started.
-
The echocardiogram looks at how well your heart is squeezing (pumping blood out) and relaxing (filling with blood), both of which are important for it to pump effectively and efficiently. Your doctor might refer to this as your ejection fraction, or EF. This is a way of calculating how much blood is pumped out of the heart with each heartbeat, and helps the medical team decide what treatment is needed. Your ejection fraction will either be reduced, mildly reduced or preserved. It is worth keeping in mind that preserved function does not always mean normal function, however this is something that a specialist heart failure doctor or nurse will be able to explain more fully if it applies to you.
-
Heart Failure cannot be cured but treatment can help to control the symptoms, improve your quality of life and slow the progression of the condition.
The treatment you receive will depend on factors such as your ejection fraction, the cause of your heart failure and your other medical conditions, but in general the following treatment might be offered:
- Medication. Most patients living with heart failure are prescribed medication to protect and enhance heart function, alleviate symptoms, and reduce fluid retention. These medications are usually started by specialist heart failure nurses who are experts getting heart failure patients on the correct medication at the correct doses for them. You can find more detailed information about common types of heart failure medication, treatments and procedures on the NHS website. Heart failure - Treatment - NHS (www.nhs.uk)
- Cardiac rehabilitation. Delivered by specialist nurses and physiotherapists, cardiac rehabilitation can help you safely increase your activity levels, improving your fitness and quality of life.
- Lifestyle changes. Heart failure specialist nurses will give advice about important lifestyle changes, such as stopping smoking, alcohol intake, diet, weight management, keeping active and getting seasonal vaccinations.
Find out more about lifestyle changes you can make to keep healthy:- Eat a balanced diet
- Keep physically active
- Watch your weight
- Stop smoking
- Moderate your alcohol intake
- Manage your stress levels
- Get enough sleep
-
It is important that you monitor your symptoms and learn to recognise changes in their pattern. Changes in symptoms may be a sign that your heart failure is worsening, so you should see your GP or specialist heart failure team.
For example, sudden weight gain could indicate fluid build-up in your body that needs treatment. You can monitor this by weighing yourself at the same time each morning.
You should follow any advice given to you by your doctor or specialist nurse, such as monitoring your daily fluid intake.
-
There is currently no cure for heart failure. It is a long-term condition, and it can be difficult to determine how it will progress for one individual, as different people are affected very differently. Some people may remain stable for many years, while in some cases it may progress very rapidly. However, detecting heart failure early and getting the right treatment can improve outcomes and give you the best outlook.
When heart failure reaches a late stage when it is very severe, many people receive palliative care at home, in a hospice or in hospital which can provide support for them and their family to make them as comfortable as possible at the end of their life.
If you or someone you care about has been diagnosed with heart failure, this can be very scary and distressing to think about or discuss. Read on below to find out more about how our compassionate Care Services team support you through this.
Find out more about our Cardiac Support Services.









